Flow Cytometry in Clinical Trials: A Powerful and Versatile Tool

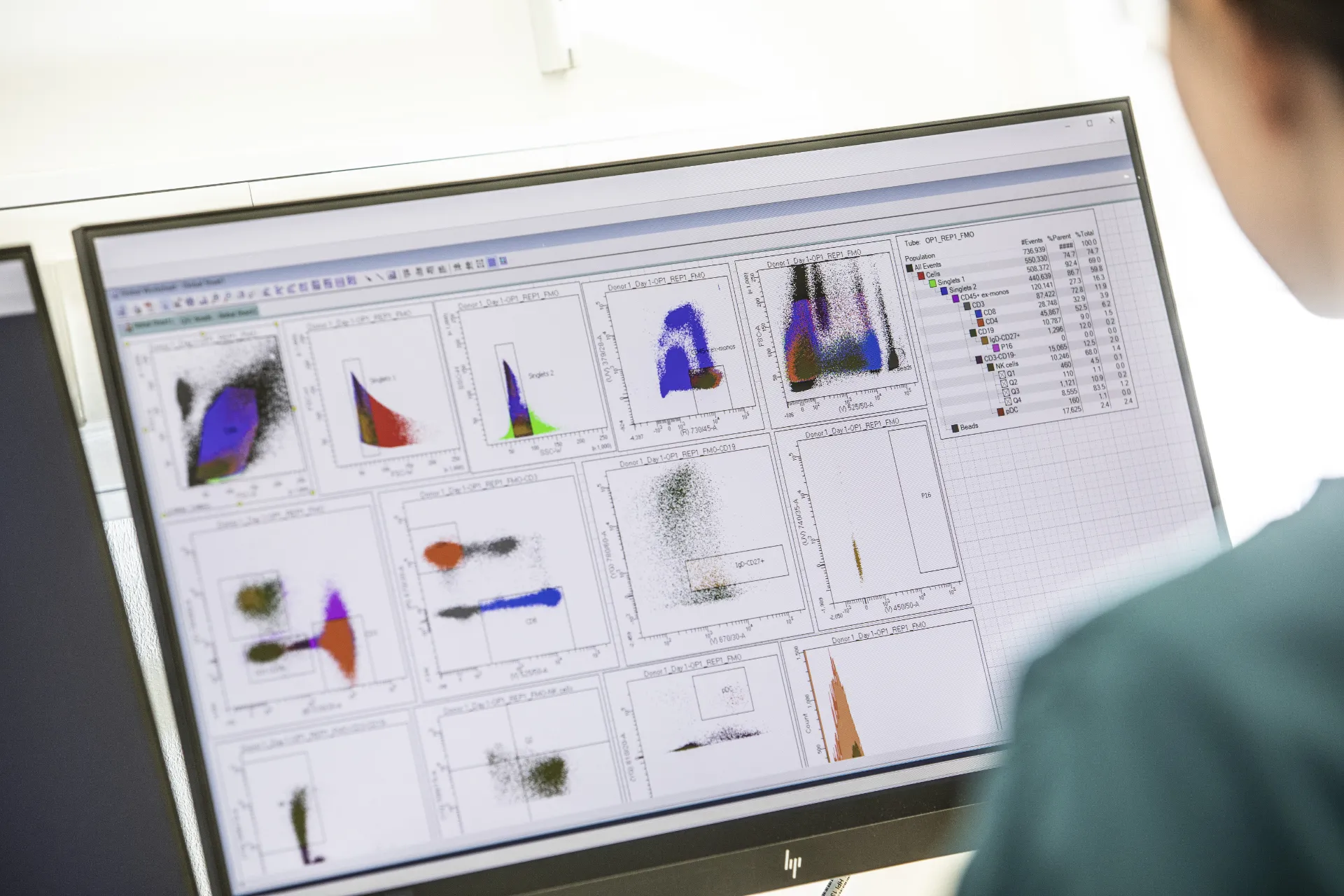
Flow cytometry is a critical tool in clinical trial sample analysis. Versatile and powerful, the breadth and richness of information it can provide can increase a project’s efficiencies and accelerate drug development. From biomarker identification to drug efficacy assessments, from functional assays to cell proliferation and viability testing, flow cytometry provides valuable insights into the cellular responses to treatment. The ability to analyse multiple parameters simultaneously at the single-cell level makes flow cytometry a key technology for researchers and clinicians working in clinical research.
ASSESSING PHARMACODYNAMIC OUTPUT EARLY
Flow cytometry provides a versatile platform for assessing pharmacodynamic (PD) responses in clinical trials by allowing the detailed analysis of cellular changes in response to a therapeutic. Performing this analysis early in clinical trials can help determine whether a therapeutic engages its target, identify potential safety and tolerability issues, and ascertain an optimal dosage range.
PD assessments contribute to informed decision-making early in the drug development process, allowing for efficient allocation of resources, both in terms of time and cost. Providing early PD data can facilitate discussions with regulatory agencies, helping to streamline the drug approval process, and ultimately, this can accelerate development and potentially bring novel therapeutics to patients more quickly.
Flow cytometry can contribute to evaluating PD output through:
- Cellular target identification
- Receptor occupancy and target engagement
- Biomarker expression analysis
- Immunophenotyping
- Cytokine and signaling pathway analysis
- Cell cycle analysis
- Apoptosis and cell death assessment
- Functional assays (cytotoxicity, phagocytosis, and other effector functions)
- Minimal residual disease detection
- Dose-Response studies
- Time course studies
The depth of information that can be generated by flow cytometry allows for a more comprehensive assessment of treatment effects, disease dynamics, and patient responses, ultimately contributing to better-informed decisions in the development and evaluation of therapeutic interventions. Using flow cytometry, a single sample can simultaneously provide pharmacokinetic, immunogenicity, and biomarker data.
ANALYSING MINOR CELL POPULATIONS
Flow cytometry enables the identification and characterisation of specific cell subpopulations based on surface markers or functional characteristics, which is crucial for understanding the heterogeneity of cellular responses in clinical samples. Furthermore, the technology can detect and quantify rare cell populations, such as circulating tumor cells or minimal residual disease in cancer patients.
This enhances the sensitivity of clinical trials in monitoring disease progression and treatment responses. Immunophenotyping using flow cytometry provides detailed information about immune cell subsets, their activation status, and functional profiles, which is essential for evaluating the impact of immunotherapies and assessing the immune response, whether it is by design or an off-target effect. However, the utility of flow cytometry can be hampered by limitations associated with the sampling and handling of whole blood. Analysing whole blood, as opposed to isolated Peripheral Blood Mononuclear Cells (PBMCs), in clinical trials can offer some efficiencies in analysis. When fresh whole blood analysis is needed, the inclusion of red blood cells provides insight into complex interactions among cell types, analysing whole blood can generally be more time and cost-efficient compared to labor-intensive isolation of PBMCs that may result in sample loss or changes in cell behaviour.
Certain analyses must be performed promptly to obtain accurate results and whole blood samples can have limited stability. Delayed processing or storage under suboptimal conditions may compromise the integrity of samples. Additionally, whole blood samples are more prone to cellular activation during handling, transportation, or storage; have the potential to clot; and may have enzymatic reactions and assays inhibited or influenced by the presence of various blood components. This can be mitigated by performing assays quickly by an in-country laboratory with expertise in handling and analysing whole blood, and in flow cytometry-based assays. 360biolabs can provide these specialised services in Australia for clinical trials in Australia – meaning samples do not need to be shipped outside of the country for analysis. Not only does this preserve the integrity of samples to ensure accurate data, but it also saves on shipping, time, and resources costs.

360BIOLABS – EXPERTS IN FLOW CYTOMETRY
Flow cytometry is a valuable and widely used tool in clinical trials, with its multiparametric approach and versatility. Continued advancements in technology; standardisation efforts; sample handling, processing, and storage; and increased collaboration among researchers and clinicians are helping to enhance the reliability and utility of flow cytometry in clinical research.
As a world-leading authority in the field of flow cytometry, immunogenicity testing, large and small molecule PK, biomarkers, cell-based assays and virology, 360biolabs understands the nuances of bioanalysis. Our immunology experts offer comprehensive analytical support for complex biologics, extensive immune monitoring capabilities and the flexibility to develop assays for new technologies, which may include delivering assays measuring specific or customised panels via flow cytometry.
We have a diverse service offering at 360biolabs in Australia, and in our North America and European laboratories. Utilising a bioanalytical laboratory with locations across the globe ensures that our clients can remain with the same high-quality laboratory as they progress their programs successfully from Phase 1 to Phase 2 and beyond.
To hear about how 360biolabs, a BioAgilytix company, can support your clinical programs contact us.
